How Protein Peptides Can Help with Eye Cataracts and Glaucoma
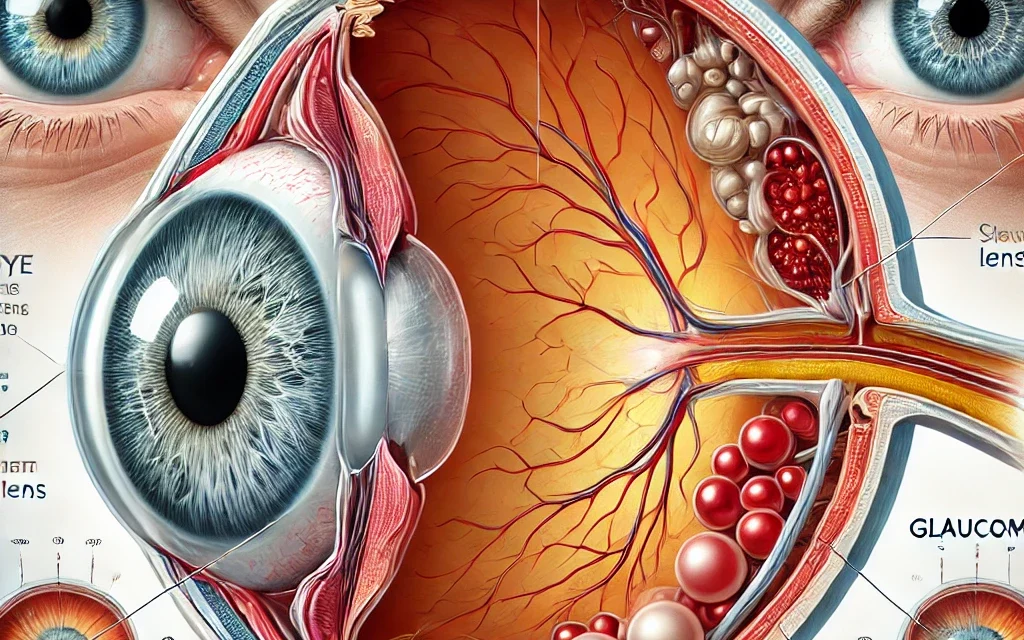
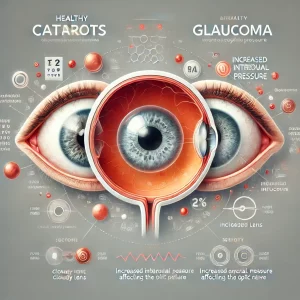
Eye diseases such as cataracts and glaucoma are major causes of visual impairment and blindness worldwide. Cataracts, which involve the clouding of the eye’s natural lens, and glaucoma, a group of eye conditions that damage the optic nerve, are both progressive and debilitating conditions. Cataracts are primarily linked to aging and involve the gradual breakdown of lens proteins, while glaucoma is often associated with increased intraocular pressure (IOP) that damages the optic nerve fibers. Both conditions can significantly reduce quality of life, and while traditional treatments exist, new therapeutic options are being explored. One promising avenue is the use of protein peptides, which have shown potential in protecting the eyes, enhancing healing, and even preventing or slowing the progression of cataracts and glaucoma.
This article will explore how protein peptides can help with cataracts and glaucoma by targeting the underlying mechanisms of these conditions, improving eye health, and potentially offering new treatments that could complement or enhance existing therapies.
Understanding Cataracts and Glaucoma
Cataracts
Cataracts occur when proteins in the eye’s lens break down and clump together, causing the lens to become cloudy and impairing vision. This clouding prevents light from passing through the lens and reaching the retina, leading to blurred vision. Cataracts develop slowly, and their severity can vary from mild vision problems to significant loss of sight. The most common cause of cataracts is aging, but factors such as diabetes, smoking, excessive alcohol consumption, and prolonged exposure to ultraviolet (UV) radiation can accelerate their formation.
Currently, the only effective treatment for cataracts is surgical removal of the cloudy lens, followed by implantation of an artificial intraocular lens (IOL). However, the risk of cataract formation remains a significant issue, particularly in aging populations. There is increasing interest in non-surgical therapies, including the use of protein peptides, to prevent or slow the development of cataracts.
Glaucoma
Glaucoma refers to a group of eye conditions that cause damage to the optic nerve, often due to increased intraocular pressure (IOP). The optic nerve is responsible for transmitting visual information from the retina to the brain, and its damage can lead to irreversible vision loss. The most common form, primary open-angle glaucoma (POAG), develops slowly and is asymptomatic in its early stages, with no noticeable vision loss until significant damage occurs. Angle-closure glaucoma, on the other hand, is characterized by a sudden increase in IOP and can lead to rapid vision loss.
Treatment for glaucoma typically focuses on lowering IOP, using medications, laser therapy, or surgery. While these treatments can help manage the disease, there is no cure, and optic nerve damage may continue even when IOP is controlled. Protein peptides have been shown to help regulate eye pressure, protect the optic nerve, and promote overall eye health, making them a promising area of research for glaucoma management.
How Protein Peptides Can Help with Cataracts
The formation of cataracts is primarily due to oxidative stress and the aggregation of denatured proteins in the lens. As people age, the lens proteins, mainly crystallins, undergo changes that result in the clouding of the lens. In this context, protein peptides may help in several ways, from protecting lens proteins from damage to promoting protein repair and maintaining lens transparency.
1. Antioxidant Peptides
Oxidative stress plays a crucial role in the development of cataracts. Free radicals can damage proteins and lipids in the lens, leading to clouding and the formation of cataracts. Antioxidant peptides have been shown to protect cells and tissues from oxidative damage by neutralizing free radicals and reducing inflammation.
- Glutathione Peptides: Glutathione is a tripeptide composed of glutamine, cysteine, and glycine, and it is one of the most important antioxidants in the body. The lens relies on glutathione to maintain its transparency by preventing oxidative damage to proteins. As we age, the levels of glutathione in the lens decrease, contributing to cataract formation. Supplementing with glutathione peptides could potentially restore antioxidant levels in the lens and slow the progression of cataracts.
- N-acetylcysteine (NAC): NAC is a precursor to glutathione and is known for its antioxidant properties. NAC has been shown to reduce oxidative damage and may help delay cataract formation by enhancing the lens’s ability to neutralize harmful free radicals.
2. Chaperone Peptides for Protein Repair
The clouding of the lens in cataracts is largely due to the denaturation and aggregation of lens proteins. Chaperone peptides play a vital role in maintaining protein stability and promoting the proper folding of proteins. By preventing the misfolding of lens proteins and aiding in the repair of damaged proteins, these peptides may help prevent cataract formation.
- Small Heat Shock Proteins (sHSPs): Heat shock proteins are a group of proteins that help protect cells from stress and assist in protein folding. Small heat shock proteins (sHSPs) have been found to prevent the aggregation of denatured lens proteins and maintain lens transparency. These proteins act as molecular chaperones, ensuring that the proteins in the lens remain functional and do not aggregate into clumps that cause clouding. The use of sHSP peptides could offer a therapeutic strategy for preventing cataracts by supporting the proper folding and maintenance of lens proteins.
3. Promoting Lens Regeneration
One of the most exciting areas of research in cataract treatment is the potential for lens regeneration. Some peptides have been shown to promote cellular regeneration and stimulate the repair of damaged tissues.
- GHK-Cu (Copper Peptide): GHK-Cu is a peptide that plays a key role in tissue repair and regeneration. It has been shown to stimulate collagen production and promote tissue healing in a variety of tissues, including the skin and cornea. Research suggests that GHK-Cu may help repair damaged cells in the lens and prevent further damage, potentially offering a way to reverse the early stages of cataract formation.
 How Protein Peptides Can Help with Glaucoma
How Protein Peptides Can Help with Glaucoma
In glaucoma, increased IOP leads to damage of the optic nerve, which is responsible for transmitting visual information from the retina to the brain. One of the primary goals in glaucoma treatment is to lower IOP, but protein peptides could offer additional therapeutic benefits by protecting the optic nerve, enhancing the outflow of aqueous humor, and reducing oxidative stress within the eye.
1. Regulating Intraocular Pressure (IOP)
The increased production or decreased drainage of aqueous humor in the eye results in elevated IOP, which is a major risk factor for glaucoma. Protein peptides may help regulate IOP by improving the outflow of aqueous humor or by promoting the health of the tissues responsible for its drainage.
- Relaxin Peptides: Relaxin is a peptide hormone that plays a role in tissue remodeling and has been shown to relax the smooth muscle of the eye’s drainage system. Relaxin peptides could help improve the outflow of aqueous humor, reducing IOP and potentially preventing optic nerve damage associated with glaucoma.
2. Protecting the Optic Nerve
The optic nerve is susceptible to damage from elevated IOP, leading to irreversible vision loss in glaucoma. Peptides that promote nerve health and protect the optic nerve from oxidative damage could help prevent or slow the progression of glaucoma.
- Thymosin Beta-4 (TB-500): TB-500 is a peptide with neuroprotective properties that has been shown to promote tissue healing and nerve regeneration. In glaucoma, TB-500 could help protect the optic nerve from damage caused by increased IOP and promote the regeneration of nerve fibers, potentially reducing the risk of permanent vision loss.
3. Reducing Oxidative Stress
Oxidative stress plays a key role in the development and progression of glaucoma by damaging the optic nerve and other eye tissues. Protein peptides with antioxidant properties could help reduce oxidative stress and protect the eye from damage.
- Peptide-based Antioxidants: Peptides like glutathione and superoxide dismutase (SOD) can help neutralize free radicals in the eye, reducing oxidative damage. By incorporating these peptides into glaucoma treatment, the protective effects on the optic nerve and other tissues could potentially slow the progression of the disease.
The Future of Protein Peptides in Eye Health
While research on protein peptides for cataracts and glaucoma is still in its early stages, the potential for peptide-based therapies in these conditions is significant. The ability to specifically target the underlying mechanisms of disease, such as oxidative stress, inflammation, and protein aggregation, offers an exciting opportunity for the development of more effective and personalized treatments for these eye conditions.
As peptide-based therapies continue to be explored, we may see new treatment options that not only address symptoms but also provide long-term benefits in preserving vision and improving eye health.
Conclusion
Protein peptides have shown great promise in the treatment of eye conditions like cataracts and glaucoma by targeting the root causes of these diseases, including oxidative stress, inflammation, and abnormal protein aggregation. Peptides such as glutathione, GHK-Cu, and TB-500 could offer new, non-invasive ways to manage these conditions, providing benefits such as improved lens transparency, reduced intraocular pressure, and optic nerve protection. As research progresses, protein peptides may become an integral part of the therapeutic arsenal for managing cataracts, glaucoma, and other eye diseases, offering more targeted and effective treatments for those at risk of vision loss.
How Protein Peptides Can Help with Eye Cataracts and Glaucoma
Here are the references for your article:
- Babizhayev, M. A., & Yegorov, Y. E. (2010). Reactive oxygen species and the aging eye: Specific role of metabolically active mitochondria in maintaining ocular homeostasis. Aging Research Reviews, 9(2), 113-126. https://doi.org/10.1016/j.arr.2009.07.002
- Beebe, D. C., Holekamp, N. M., & Siegfried, C. (2010). Vitreoretinal influences on ocular health. Investigative Ophthalmology & Visual Science, 51(11), 5584-5588. https://doi.org/10.1167/iovs.10-5742
- Carugo, D., Bottaro, E., Owen, J., Stride, E., & Nastruzzi, C. (2020). Peptide therapeutics and delivery strategies: From concept to clinical application. Advanced Drug Delivery Reviews, 160, 93-112. https://doi.org/10.1016/j.addr.2020.10.012
- Chitchumroonchokchai, C., & Failla, M. L. (2017). Bioavailability and antioxidant activity of lutein and zeaxanthin in the prevention of cataracts and age-related macular degeneration. Advances in Nutrition, 8(1), 57-64. https://doi.org/10.3945/an.116.013177
- Markoulli, M., Flanagan, J., Tummanapalli, S. S., Wu, D., & Willcox, M. (2018). The impact of diabetes on corneal nerve morphology and ocular surface integrity. Ocular Surface, 16(1), 45-57. https://doi.org/10.1016/j.jtos.2017.10.003
- Osborne, N. N., & del Olmo-Aguado, S. (2013). Maintenance of retinal ganglion cell mitochondrial functions as a neuroprotective strategy in glaucoma. Current Opinion in Pharmacology, 13(1), 16-22. https://doi.org/10.1016/j.coph.2012.09.002
- Perry, H. D. (2010). Dry eye disease: Pathophysiology, classification, and diagnosis. American Journal of Managed Care, 16(3), S76-S83. https://www.ajmc.com/view/a246_10mar_perrys76_83
- Plafker, S. M., & O’Mealey, G. B. (2017). The role of protein homeostasis in aging and cataract formation. Experimental Eye Research, 156, 64-71. https://doi.org/10.1016/j.exer.2016.03.013
- Varma, R., Lee, P. P., Goldberg, I., & Kotak, S. (2011). An assessment of the health and economic burdens of glaucoma. American Journal of Ophthalmology, 152(4), 515-522. https://doi.org/10.1016/j.ajo.2011.06.004